The large number of fraudulent activities in healthcare; increasing number of patients seeking health insurance; the prepayment review model; growing pressure of fraud, waste, and abuse on healthcare spending; and high returns on investment.
Market Size
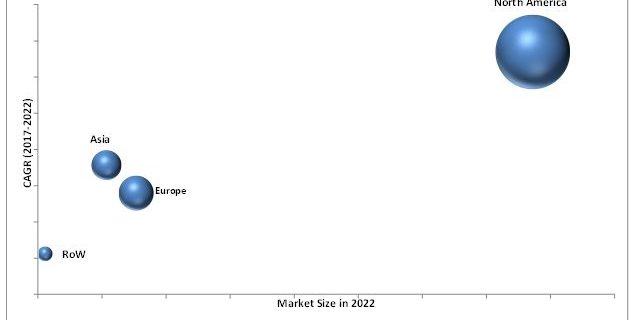
The global Healthcare Fraud Detection market size is projected to reach USD 2,242.7 Million by 2022 from USD 631.0 Million in 2017, at a CAGR of 28.9%.
IBM (US), Optum (US), SAS (US), McKesson (US), SCIO (US), Verscend (US), Wipro (India), Conduent (US), HCL (India), CGI (Canada), DXC (US), Northrop Grumman (US), LexisNexis (US), and Pondera (US) are some key players in this market. These companies are focusing on increasing their presence in the high-growth markets through both organic as well as inorganic growth strategies such as product launches, acquisitions, and expansions.
For More Details, Download a PDF Brochure:-
https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
“IBM is a leading player in the healthcare fraud detection market”
The leading position of the company is attributed to its robust product portfolio. The company offers exhaustive healthcare fraud analytic solutions for application in healthcare. The company has a strong presence in the commercial and government healthcare payer markets. For instance, since 2005, the company has invested USD 24 billion in the development of its Big Data and Analytics software and services capabilities. For instance, in April 2016, IBM acquired Truven (US), a provider of cloud-based healthcare data, analytics, and insights.
“McKesson held the second position in the market among the leading players in 2016”
The company has a strong presence in the US and Canadian markets. It has a strong customer base including more than 300 payer customers. The company focuses on inorganic growth strategies to strengthen its position in the market. In this regard, in February 2016, McKesson agreed with HealthQX (US) to help payers quickly design and scale complex bundled payment models and help ensure those innovative programs provide timely and accurate payment to providers.
We can help with your specific research requirement for this market. Please share your specific interest to help us serve you better, Request Sample Pages:-
https://www.marketsandmarkets.com/requestsampleNew.asp?id=221837663


